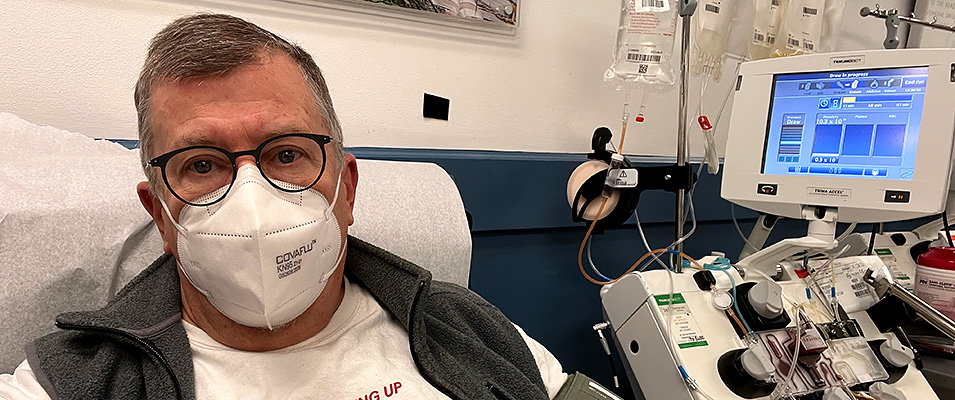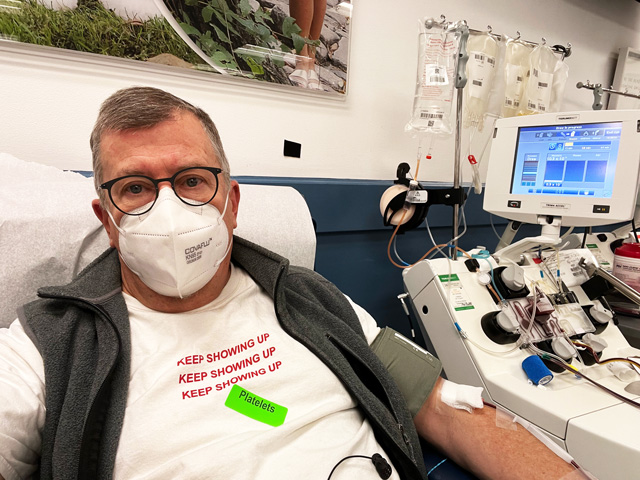
Todd Wilson donates platelets.
By Giulia Gionta
Nearing the end of 2021, amid the second year of the ongoing COVID-19 pandemic, American hospitals are in dire need of blood. The blood supply in the United States is dangerously low, according to the American Red Cross. “Throughout the pandemic, we have experienced challenges collecting blood for patients from blood drive cancellations to surging hospital demand,” said Chris Hrouda, president of Red Cross Biomedical Services. “Now with decreased blood donor turnout, our Red Cross blood supply has dropped to the lowest it has been at this time of year since 2015.”
Without stable blood supplies, hospitals nationwide may be forced to alter treatments for patients, or cancel patients’ surgeries. Each day, life-saving blood transfusions are needed in hospitals and emergency treatment facilities across the U.S.
Dr. Jennifer Andrews, a pediatric hematologist and blood bank director for Vanderbilt University Medical Center in Nashville, explained what a blood shortage entails. “From a practical standpoint, a blood shortage means that at times we might have to prioritize patients,” says Andrews. “So, who needs the transfusion more than another one of our patients. Unfortunately, we’ve had to defer patients for major surgeries and delay blood transfusions for people that could afford to wait a little longer.”
The COVID-19 pandemic may be to blame for this abnormal blood donor shortage. Some blood collection organizations are having to cancel blood drives in schools and businesses due to precautionary pandemic procedures limiting the number of individuals allowed onsite.
Blood donations are crucial because blood, platelets, and plasma cannot be manufactured in a laboratory. While 38% of the American population is eligible to give blood, only 2% actually donates.
A Statista poll in August of 2021 showed a decrease in the number of adult blood donors across the U.S. from 2001 to 2020. In 2020, 13% of eligible adults donated blood, whereas in comparison, 21% of eligible adults donated blood in 2001.
“I’ve been donating blood for almost 40 years regularly,” says Todd A.Wilson, Strategic Communications Director at Adelphi University. “Every year since I turned 18, a few times each year. For the last five years, I’ve donated platelets about every three weeks -- more than 80 of those to date.”
According to the New York Blood Center’s official website, close to 2,000 donations are needed each day in the New York and New Jersey community for patients who require lifesaving blood or platelet transfusions. Those in need include but are not limited to patients that are suffering from cancer, accidents, or burns. Newborn babies and mothers, transplant recipients, surgery patients, and patients suffering from sickle cell disease also require transfusions.
“Because we never know what’s coming, we always have to have enough blood supply to save someone’s life,” Andrews says. “We need consistent blood supply on a daily basis for us to do our regular business at the hospital. We are always in short supply of blood platelets, and we always are in need of type O red blood cells. There are two universal blood types, O positive and O negative. We use these for every trauma patient because in the moment we don’t have enough time to figure out what blood type the patient is, so we have to give them type O.”
Minority donors, such as Hispanics, Asians and African Americans, have rare compatibility traits in their blood that are unique to their ethnicity. Therefore, optimal blood matches for minority patients will come from donors with their same ethnic background. Sickle cell disease is an inherited red blood cell disorder where there are not enough healthy red blood cells to carry oxygen throughout the body. Also known as sickle cell anemia, it causes infection and pain in people affected.
On average, sickle cell disease patients rely on 15-25 blood transfusions per year. Without compatible trait blood transfusions, the patient can develop antibodies and build tolerance to the blood they receive, which leads to further complications and more necessary blood transfusions.
According to Inova Blood Donor Services, sickle cell anemia occurs in 1 out of every 500 African American births, and the sickle cell trait occurs in about 1 in 12 African Americans.
Throughout September and October, there have been reports of less than a day’s supply of certain blood types collected by the American Red Cross. To replenish inventory adequately, the Red Cross’s goal was to collect 10,000 additional blood products each week of October to meet hospital and patient needs.
There are a few common reasons that may require donors to temporarily defer giving blood. If donors are sick or ill, they must wait until they are feeling completely better to make a donation. While most medications will not prevent them from donating, some may require a waiting period after a final dose. If donors are anemic or have low iron they cannot donate, but boosting iron levels is possible to make them eligible to donate. Finally, if donors have traveled outside of the U.S. and Canada within the past three years, they will be questioned for travel details to determine their eligibility in donating blood.
A poll published by Statista in February 2021 reveals the number of blood donor deferrals in the U.S. in 2017 by reason and gender. In 2017, there were an estimated 862,000 blood donor deferrals among males in the United States. The most common reason for donor deferral among both males and females was low hemoglobin/hematocrit. The overall number of total deferrals was higher among females at 1,683 and males deferred at 862.
“I remember way back when I was 18 and first gave blood,” says Wilson. “I got dizzy the first couple times after donating. I had to lay down and elevate my feet and keep an ice pack nearby, but that’s fairly typical for first time donors. After several times of donating, your body realizes you’ll be okay.”
Donating blood is simple and safe. Amanda Pietro, a volunteer of the American Red Cross for six years in New Jersey, stresses the safety measures her and fellow volunteers adhere to at blood drives and clinics, especially amid the COVID-19 pandemic. “We wear all necessary PPE and sanitize surfaces still between our donors," says Pietro. "Our equipment is sterile and only used once, then disposed of.” There is no danger in contracting transmissible infectious disease, such as HIV/AIDS, by donating blood.
Data collected on the number of blood transfusions in the U.S., comparing 2005 to 2017 by location, reveals that in 2017 there were approximately 1,042,000 red blood cell transfusions in emergency settings across the U.S., closely compared with 1,007,000 red blood cell transfusions in the same settings in 2005. But the current quantity of blood supply is not meeting demands across the U.S., and blood is being used in hospitals faster than donations are coming in.
Historically, this time of year is typically when blood supplies are lowest due to how busy people become around the holidays.“Maybe for the holidays this year you can donate blood for your community," Andrews suggests. "Start a new family tradition and donate for people who need it.”